Safe Haven Baby Boxes are implemented with the goal of preventing illegal abandonment of newborn children. Not only is the Baby Box offered as a last resort option for women, maintained with complete anonymity, but the organization itself raises awareness and offers a 24 hour hotline for mothers in crisis.
/cloudfront-us-east-1.images.arcpublishing.com/gray/JMMBCOND55FANAKEWYAZSFCEAA.jpg) |
| Safe Haven Baby Box |
The primary goal of Safe Haven Baby Boxes is to raise awareness of the Safe Haven Law. These laws vary across states, in areas such as maximum age at which an infant can be relinquished, whom can relinquish the infant, and where the relinquishment can occur, but overall provide safe places for parents to relinquish their newborn infants. It provides anonymity and protection against prosecution for the infant's caretakers as well as immunity of liability for providers who accept the infants. All fifty states and Puerto Rico have some variation of the Safe Haven Law. The first state to enact this type of law was Texas, who in 1999 created their "Baby Moses Law." This laws was created in a reaction to thirteen incidents of child abandonment that year, with three of the infants being discovered dead. Kentucky's version of this law is the Safe Infants Act, which allows parents to leave babies younger than 30 days old at a designated safe place, where no one will call the police or ask for your name. The baby will get medical care and be placed with a family for adoption. If the parents of the infant do not contact the Cabinet for Health and Family Services within 30 days after leaving the infant at a safe place, the Cabinet will begin the process of terminating parental rights. The World Population Review provides a breakdown for the law by each state.
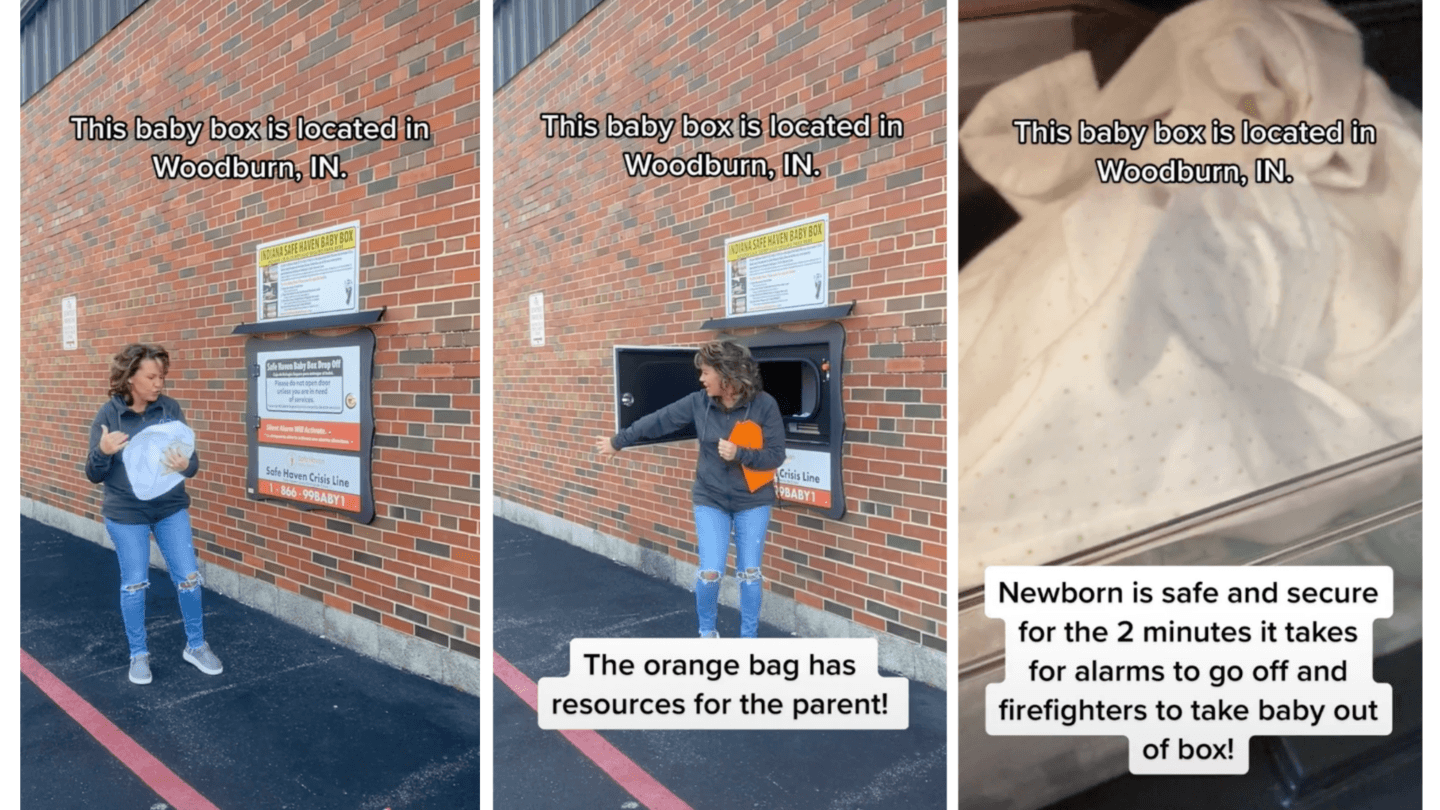 |
| Viral TikTok Shows How Safe Haven Baby Boxes Work |




 NPR: James Gathany
NPR: James Gathany Cambridge Independent: Malaria kills a child every two minutes - and now mosquitoes are becoming resistant to insecticide
Cambridge Independent: Malaria kills a child every two minutes - and now mosquitoes are becoming resistant to insecticide  A baby in Kenya sleeps under an insecticide-treated bed net.SVEN TORFINN/WHO/PANOS PICTURES/REDUX
A baby in Kenya sleeps under an insecticide-treated bed net.SVEN TORFINN/WHO/PANOS PICTURES/REDUX